Medical billing is a critical component of any healthcare specialty, but cardiology medical billing presents unique challenges due to its complex procedures, extensive documentation, and evolving insurance regulations. From diagnostic tests like echocardiograms to interventional procedures such as stent placements, every service requires precise coding and compliance with payer policies. Without an optimized cardiology billing process, practices risk revenue losses, claim denials, and compliance issues.
This guide will break down the cardiology billing process, highlight best practices for cardiology revenue cycle management, and provide insights on medical coding for cardiology, denial management, and the role of automation in improving accuracy and efficiency.
What is Cardiology Medical Billing
Cardiology medical billing refers to the systematic process of submitting and managing claims for cardiovascular procedures, ensuring that healthcare providers receive proper reimbursements. Unlike general medical billing, cardiology billing services require a deep understanding of ICD-10 coding for cardiology, CPT codes for cardiology procedures, and payer-specific rules.
Errors in cardiology coding and billing can lead to delayed reimbursements, increased denials, and even compliance violations. To mitigate these risks, medical billing for cardiology practices must incorporate accurate patient eligibility verification, thorough documentation, and proper claim submission protocols.
Key Steps in the Cardiology Billing Process
A structured cardiology revenue cycle management (RCM) process ensures that healthcare providers receive payments for services rendered while maintaining regulatory compliance. Below are the essential steps:
1. Patient Registration & Eligibility Verification
Before rendering any cardiology services, it’s essential to verify the patient’s insurance eligibility. This step ensures that treatments such as angioplasty, echocardiograms, or stress tests are covered under the patient’s plan. Failure to verify eligibility can result in claim rejections, increasing administrative burdens.
2. Medical Coding for Cardiology
Cardiology coding and billing require precise documentation using:
-
ICD-10 codes for cardiology diagnoses (e.g., I25.10 for coronary artery disease).
-
CPT codes for cardiology procedures (e.g., 93000 for electrocardiogram interpretation).
-
HCPCS codes for supplies and services used during treatment.
Improper medical coding for cardiology can lead to claim denials or audits by Medicare and private insurers.
3. Claims Submission & Reimbursement
Once coding is complete, claims are submitted to payers like Medicare, Medicaid, or private insurance companies. Practices must ensure that documentation aligns with payer requirements to avoid delays in reimbursements.
4. Denial Management & Appeals
Claim denials in cardiology billing services can occur due to incorrect coding, lack of documentation, or missing prior authorizations. A robust denial management process ensures that rejected claims are corrected and resubmitted promptly.
- Read: Wound Care Billing | Orthopedic Billing
Common CPT Codes for Cardiology Billing
Accurate coding is crucial for cardiology billing to ensure proper reimbursement and compliance. Below is a categorized list of commonly used CPT codes in cardiology:
Echocardiography
-
Transthoracic echocardiogram (TTE) – CPT 93306
-
Transesophageal echocardiogram (TEE) – CPT 93312
-
Stress echocardiogram – CPT 93350
Electrocardiography (ECG/EKG)
-
Routine electrocardiogram (ECG) with at least 12 leads – CPT 93000
-
Holter monitoring (24-hour ECG recording) – CPT 93224
-
Event monitoring (30-day ECG recording) – CPT 93268
Cardiac Catheterization
-
Left heart catheterization with coronary angiography – CPT 93458
-
Right heart catheterization – CPT 93530
-
Coronary angioplasty with stent placement – CPT 92928
Pacemaker & Implantable Cardioverter-Defibrillator (ICD) Procedures
-
Insertion of single-chamber pacemaker – CPT 33206
-
Insertion of single-chamber ICD – CPT 33249
-
Replacement of pacemaker pulse generator – CPT 33227
Nuclear Cardiology
-
Myocardial perfusion imaging (single study at rest or stress) – CPT 78452
-
Myocardial viability study with SPECT – CPT 78478
Cardiovascular Stress Testing
-
Exercise treadmill stress test – CPT 93015
-
Pharmacologic stress test – CPT 93017
-
Stress test with imaging (e.g., nuclear or echocardiography) – CPT varies by modality
Cardiac Rehabilitation Services
-
Supervised cardiac rehabilitation (per session) – CPT 93797
-
Medical nutrition therapy (initial assessment and intervention) – CPT 97802
Peripheral Vascular Procedures
-
Peripheral angiography (unilateral) – CPT 75710
-
Lower extremity arterial revascularization (open or percutaneous) – CPT 37221
Compliance & Regulations in Cardiology Billing
The financial success of a cardiology practice depends on strict adherence to compliance standards such as:
-
HIPAA (Health Insurance Portability and Accountability Act): Protects patient information.
-
Medicare & Medicaid Guidelines: Dictate specific reimbursement policies.
-
CMS (Centers for Medicare & Medicaid Services) Rules: Set forth coding and documentation requirements.
Failure to comply with these regulations can lead to financial penalties or legal repercussions. Medical billing for cardiology practices must include compliance audits to ensure adherence to evolving policies.
Common Challenges in Cardiology Medical Billing & Solutions
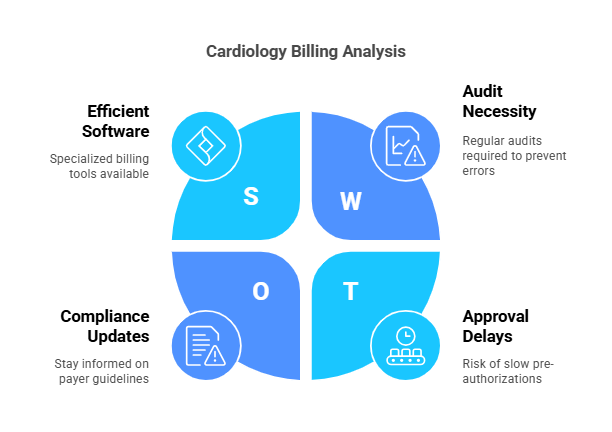
Despite following best practices, cardiology medical billing remains challenging due to frequent updates in payer guidelines, complex procedural codes, and prior authorization issues.
1. Frequent Claim Denials
Cardiology claims are often denied due to coding errors, missing documentation, or lack of medical necessity justification. The solution is to conduct pre-claim audits and utilize automated coding verification tools.
2. Complex Procedure Coding
Many cardiology procedures, such as cardiac catheterization and electrophysiology studies, require multiple codes for proper reimbursement. To manage this, practices should invest in specialized cardiology billing software that automatically cross-references codes.
3. Prior Authorization Issues
Insurance companies often require pre-authorizations for high-cost cardiology treatments like stent placements or nuclear stress tests. Streamlining this process through automated eligibility verification tools can reduce delays.
Read:
| Cardiology Medical Billing 101 |
| Orthopedic Medical Billing 101 |
| Radiology Medical Billing 101 |
| Orthotics Medical Billing 101 |
| Phsycian Medical Billing 101 |
The Role of AI & Automation in Cardiology Billing
With advancements in technology, AI-driven cardiology billing software is revolutionizing the cardiology revenue cycle management process. These tools help:
-
Reduce medical coding errors through automated code matching.
-
Speed up claims submission by detecting missing information.
-
Optimize denial management by analyzing patterns in claim rejections.
By integrating AI into cardiology billing services, practices can improve efficiency and minimize revenue loss.
- Read our complete guide on: Medical Billing Time Limits by State
What Are the Top 6 Unexpected Cardiology Billing Denials & How to Prevent Them?
Billing denials can disrupt cash flow and delay reimbursements for cardiology practices. Below are six common but unexpected reasons for denials, along with solutions to prevent them.
1. Missing or Incorrect Patient Information
Errors in demographic details, insurance ID numbers, or patient data can lead to automatic claim rejections. Even minor mistakes, like a misspelled name or incorrect birthdate, can result in denials. Implement a verification system to ensure accuracy before claim submission.
🔹 Solution: Implement a verification checklist at patient intake to confirm all details before submission. Utilize automated eligibility verification tools to cross-check patient information against payer databases.
2. Lack of Preauthorization
Many cardiology procedures require prior authorization from insurance providers. Failure to obtain it can result in claim denials or delayed payments. Ensure your team checks preauthorization requirements before scheduling tests or procedures and submits requests early.
🔹 Solution: Set up a preauthorization workflow where staff checks requirements before scheduling procedures. Use real-time insurance portals to submit and track preauthorization requests efficiently.
3. Illegible or Improperly Formatted Claims
Illegible handwriting, incomplete electronic submissions, or incorrect formatting can lead to processing errors. Use EHR (Electronic Health Record) systems or practice management software to standardize and automate claim submissions, reducing the risk of rejection.
🔹 Solution: Use EHR (Electronic Health Records) or practice management software to generate and submit claims electronically. Conduct routine audits to ensure claims meet payer formatting standards before submission.
4. Duplicate Claim Submissions
Resubmitting claims without checking the status of the original can trigger denials for duplication. To avoid this, track each claim’s submission and response status carefully. Implement a system that flags potential duplicate submissions before processing.
🔹 Solution: Implement a claim tracking system to monitor submission status. Train billing staff to check denial codes before resubmitting a claim and avoid unnecessary duplicate submissions.
5. Insufficient Medical Necessity Documentation
Insurance companies often deny claims if there’s inadequate justification for a procedure or test. Ensure thorough documentation, including physician notes, test results, and medical history, to clearly support the medical necessity of each service provided.
🔹 Solution: Ensure thorough physician documentation, including test results, patient history, and physician notes. Use EHR templates that prompt providers to include necessary supporting details for each procedure.
6. Non-Covered Services
Certain cardiology procedures may not be covered under a patient’s insurance plan. Verifying coverage before performing a procedure is essential to avoid denials. Inform patients in advance about potential out-of-pocket costs and obtain written consent when necessary.
🔹 Solution: Verify coverage before performing the procedure using insurance eligibility checks. Inform patients of potential out-of-pocket costs and obtain written consent for non-covered services to prevent disputes.
Best Practices for Efficient Cardiology Billing
To ensure accuracy and timely reimbursements, follow these best practices:
-
Use a Cardiology-Specific Billing System – Invest in cardiology billing software tailored for cardiovascular procedures.
-
Stay Updated on Coding Guidelines – Regularly review ICD-10 codes for cardiology and CPT codes for cardiology procedures.
-
Conduct Regular Compliance Audits – Ensure that medical billing for cardiology practices adheres to HIPAA and CMS rules.
-
Train Staff on Cardiology Billing – Ongoing training reduces coding errors and enhances claim accuracy.
Read:
How to Reduce Cardiology Billing Claim Denials?
Cardiology billing claim denials disrupt revenue flow and delay reimbursements. Implement these targeted strategies to minimize denials and improve cash flow.
1. Streamline Denials Management
✅ Assign a dedicated team to track, investigate, and resolve claim denials.
✅ Identify root causes and implement corrective measures to prevent recurring issues.
2. Verify Preauthorization Before Procedures
✅ Confirm payer requirements before scheduling cardiology tests and procedures.
✅ Train staff to initiate preauthorization early and track approvals to prevent delays.
3. Ensure Accurate Documentation
✅ Use Electronic Health Records (EHR) for clear, legible, and complete patient documentation.
✅ Standardize provider notes to justify procedures and meet insurance requirements.
4. Strengthen Medical Coding Accuracy
✅ Provide ongoing CPT and ICD-10 coding training to reduce errors.
✅ Stay updated on cardiology-specific coding changes to ensure compliance.
5. Implement Claims Scrubbing Technology
✅ Use claims scrubbing software to detect errors, duplicate submissions, and missing data before claims are submitted.
✅ Reduce rework and speed up reimbursements with automated validation checks.
6. Verify Patient Information at Every Visit
✅ Confirm insurance details and demographic data before claim submission.
✅ Triple-check patient records to avoid denials due to missing or incorrect information.
Outsource to Quality Healthcare Systems (QHS) for Seamless Cardiology Billing
Handling cardiology billing in-house requires dedicated resources, expertise, and constant updates on regulatory changes. Outsourcing to Quality Healthcare Systems (QHS) ensures accurate claim submissions, faster reimbursements, and reduced denials.
Why Outsource to QHS?
✅ Fewer Denials, Faster Payments – Our expert billers reduce errors and resubmit denied claims promptly.
✅ Regulatory Compliance – Stay updated with coding changes and payer requirements.
✅ Lower Administrative Costs – No need for an in-house billing team, saving overhead expenses.
Challenges of In-House Billing
❌ Increased Workload – Managing claims, denials, and compliance takes time away from patient care.
❌ Higher Costs – Hiring and training billing staff adds long-term expenses.
❌ Risk of Revenue Loss – Errors in coding or documentation lead to denied claims and cash flow disruptions.
Final Thoughts on Cardiology Medical Billing
Efficient medical billing for cardiology practices is essential for financial stability. By implementing best practices, using cardiology billing software, and staying updated on ICD-10 and CPT codes for cardiology, practices can maximize reimbursements while reducing claim denials. If your practice struggles with cardiology coding and billing, consider outsourcing to specialized cardiology billing services for streamlined operations and compliance assurance.
Read: