Welcome to Quality Healthcare Systems
Your Trusted Medical Billing and Revenue Cycle Management Company
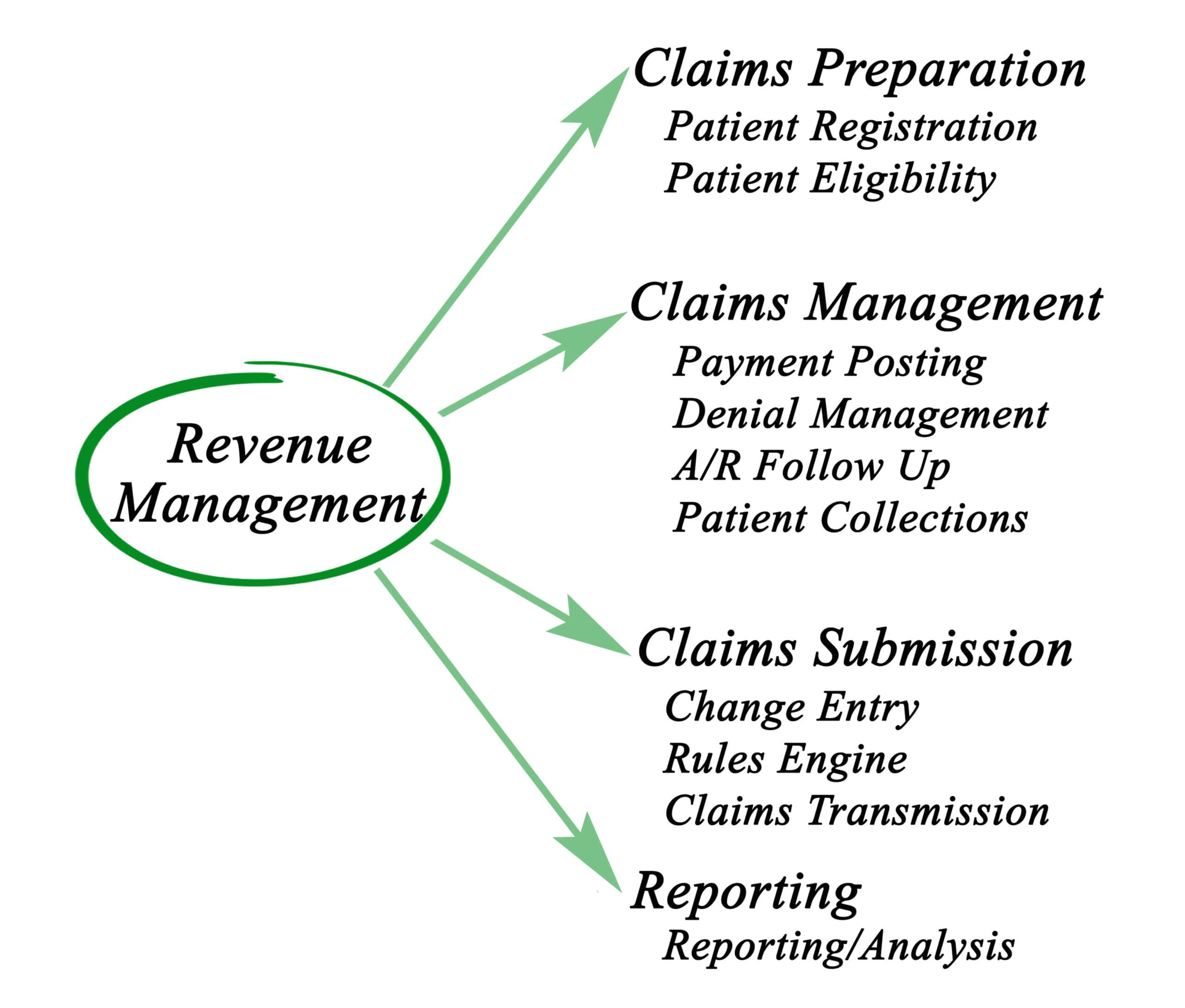
At Quality Healthcare System (QHS), we understand the unique challenges faced by small practices and medical equipment suppliers when it comes to managing billing and revenue cycles. As a leading medical billing company, we simplify the billing process and improve your financial stability. Our comprehensive services allow you to focus on delivering quality patient care while we take care of the billing details. From claims submissions to patient eligibility verification, we provide end-to-end billing solutions that reduce errors, speed up payments, and improve your cash flow.
What We Do
Custom Medical Billing Solutions to Maximize
Your Practice Revenue

QHS is dedicated to providing efficient billing solutions with a special focus on durable medical equipment (DME) billing. As a trusted DME billing company, we handle everything from patient eligibility verification to claims processing and payment collection. Whether you’re a small medical practice or a large supplier of medical equipment, our team is equipped to manage your billing needs with precision and expertise.
- Patient Eligibility Verification
- Accurate Claims Submission
- Denial Management
- Accounts Receivable (A/R) Follow-Up
- Financial Reporting
Our Process
Efficient Billing Process for Proven Results
At QHS, we use a streamlined approach to manage medical billing and revenue cycle management, making sure that every claim is processed efficiently. We aim to reduce administrative burdens on your team while increasing your practice’s revenue. Here’s how our process works
Initial Review
We begin by reviewing your current billing practices and identifying areas for improvement. Our team works closely with your practice to understand your specific needs and tailor a solution that fits your workflow.
Patient Eligibility and Insurance Verification
We make sure that every patient’s insurance is verified before services are provided. Our systematic approach minimizes the risk of unpaid claims and increases the likelihood of timely payments.
Accurate Coding and Claims Submission
Proper coding is essential for smooth claims processing. Our team accurately codes all medical services and equipment to minimize the chances of claim denials.
Claims Management
We submit your claims to the appropriate insurance companies and handle any follow-ups required to resolve issues or resubmit denied claims. Our focus is on getting your payments processed as quickly as possible.
Payment Posting and Reconciliation
We promptly post received payments to your accounts, addressing any discrepancies to maintain accurate financial records.
Ongoing Reporting and Support
We provide detailed financial reports, allowing you to monitor your practice’s cash flow, track performance, and make informed business decisions.
Our Specialties
Tailored Billing Services for Diverse Healthcare Needs
In addition to being a reliable medical billing company, QHS specializes in billing services across various medical fields. Our specialties include
- Pharmacy Billing
- Home Health Billing
- Wound Care Billing
- Orthopedic Billing
- Orthopedic Billing


99%
Satisfied Clients
For more than 15 years

Why Choose Us?
At QHS, we believe that every medical practice, no matter the size, deserves a billing partner they can rely on. Our unique approach to medical billing and revenue cycle management focuses on delivering tangible results for our clients. Here’s what makes QHS stand out
- Expertise in DME Billing: As a leading DME billing company, we understand the complexities involved in billing for durable medical equipment. Our team stays up-to-date on the latest industry changes, ensuring compliance with all regulations and best practices.
- Customized Solutions: We offer flexible billing solutions that can be customized to meet the specific needs of your practice. Whether you’re looking for full-service billing or support in specific areas, we’ve got you covered.
- Dedicated Support: Our team is committed to providing personalized service. We’re always available to answer questions, provide updates, and ensure that your practice is getting the most out of our services.
- Transparent Pricing: At QHS, we provide clear and comprehensive pricing covering all essential services. Our offerings include everything from accounts receivable processing to denied claims follow-up and timely patient statement distribution.
- Transparent Reporting: We provide regular, detailed financial reports that help you understand your practice’s financial performance and make informed decisions.
Testimonials
"QHS has exceeded our expectations with their expertise and dedication. They not only help us collect revenue efficiently but also provide valuable insights to grow our business. I highly recommend them to any healthcare company."


Contact for
Frequently Asked Questions
QHS provides expert denial management services in North Carolina and nationwide, helping healthcare providers resolve denied claims quickly.
Denial management involves reviewing denied claims, correcting errors, resubmitting claims, and following up with insurance providers until payment is received.
Denial management in AR (Accounts Receivable) calling refers to the process of addressing and resolving denied claims by communicating with insurance providers, ensuring that denied claims are corrected and paid.
QHS offers flexible pricing for denial management services, with solutions tailored to the size and needs of your practice. Contact us today to learn more about our pricing options.

Customized Medical Billing Solutions
What We Do
Durable Medical Equipment
- Commercial
- Medicaid
- Medicare
- Durable Medical Equipment Regional Carriers
- Private Payers

Outsourced Medical Billing
This service provides an outsourced business model allowing your team to use our software solutions in managing your transactions. With an inhouse billing team, you gain access to claims data and patient eligibility instantly.
Audit and Appeals Assistance
We offer audit relief service packages that provide you with the knowledge and key insights to navigate the multitude of DME audits from numerous contractors.
Patient Collections
Our all-in-one solution allows your staff to concentrate on higher payoff activities. With our complete patient collections service, you can improve efficiency and develop an upfront policy in getting paid.
Special Projects
Outsourcing your billing to QHS can have a transformative effect on your business. Here’s how
- Assisting in Open Sales Orders (Backlog of Unconfirmed Orders)
- Cleanup of Old Accounts Receivable (From All or Specific Payors, Product Lines, etc.)
- Cleanup of On-Hold Files
- Conversions of Software
- Obtaining CMNs / PARs
- Payment Posting

Denials and Rejection Analysis
Our Claims Analysts help reduce costs and improve collections by analyzing each claim on the front end. This service effectively minimizes claim rejection rates and denials to get you paid faster and remove the burden of collections and claim resubmission.

Electronic Claim Submission
Reduce time spent filling out tedious forms and help your facility get paid for the services rendered as quickly as possible by submitting your claims electronically.

How to Outsource my Billing and What Is Included?
QHS assumes all of the provider’s in-house billing staff responsibilities.
The provider will do all intake reviews for claims to be worked and submitted by QHS.
After the claim has gone through the compliance review and other intake functions, QHS will provide the following:
- Review all claims prior to submission for billing errors (ie: HCPCS codes, Modifiers etc.)
- Transmit claims (after review)
- Work front end rejections
- Work A/R and Denials
- Post payments
- Conduct calls to provide staff feedback
- Conduct executive calls and billing analysis to measure productivity
The agency you choose affects your profit, so it is important to study your options to stay ahead of the competition.


Competitive Pricing
- Accounts Receivable Processing
- Denied Claims Follow Up
- Low Ticket Claims Follow Up
- Pursuing Provider Proactively for Incomplete Information
- Timely Patient Statement Send Out
Contact Us
The Need for Specialized Billing Agencies
We have collaborated with Pedors Shoes with the billing process for providers in the diabetic footwear sector. Through an interview, company President Stephen O’Hare shared his opinion on the need for billing agencies based on his experience with his business.
Many qualified and critical Pedorthists have gone out of business due to the recession. On top of this, there were recent additions to documentation requirements for diabetic shoes and inserts that made providers discontinue the business because of their fear denials and audits. As result, patients needing diabetic shoes no longer have access to this product.
For Pedors Shoes, our expertise in DMEPOS billing can help in addressing the shortfall in the number of qualified providers which can reduce the denial of claims drastically.