Disputing a medical bill can be stressful, but knowing the right steps can help you fix errors and avoid paying more than you should. Many patients face billing mistakes, insurance claim denials, or unexpected charges, but you have the right to challenge them.
You can start by checking your Explanation of Benefits (EOB) and asking for an itemized bill to spot any errors. If you find a mistake or an unfair charge, contact your insurance company to understand why. If the issue isn’t resolved, you can file a formal dispute by sending an appeal with supporting documents like medical records, doctor’s notes, and past communication with your insurer.
In this guide, we’ll walk you through the entire process of disputing a medical bill with your insurance company, ensuring you can navigate the dispute with confidence.
Steps to Dispute Medical Bills with Insurance
Disputing a medical bill with your insurance involves a clear, step-by-step process to ensure you only pay for services rendered. Follow these steps:
- Review Your Documentation:
- Obtain your itemized bill and Explanation of Benefits (EOB).
- Compare these documents to verify that the charges match the services provided. Look for discrepancies such as duplicate charges or incorrect procedure codes.
- Gather Evidence:
- Collect all supporting documentation, including medical records, doctor’s notes, and any prior authorizations.
- Keep copies of your itemized bill and EOB for reference. For additional guidance on managing medical bills, visit the Consumer Financial Protection Bureau.
- Contact the Provider’s Billing Department:
- Reach out to your healthcare provider’s billing department to clarify any discrepancies.
- Request an explanation and, if necessary, a corrected bill. Document all communications with dates, times, and the names of representatives.
- File a Formal Dispute with Your Insurer:
- If the provider’s response is unsatisfactory, submit a formal dispute or appeal with your insurance company.
- Include all supporting evidence and clearly explain the errors, referencing specific charges. For assistance in navigating the dispute process, consider visiting the Patient Advocate Foundation.
- Follow Up and Escalate:
- Regularly follow up with both your provider and insurer regarding the status of your dispute.
- If the issue remains unresolved, escalate by contacting your state’s insurance department through the National Association of Insurance Commissioners (NAIC).
- You may also seek help from a patient advocate if necessary.
- Read: Types of DME
How to Negotiate a Medical Bill with Insurance
If disputing the bill doesn’t work, try negotiating directly with your healthcare provider or hospital billing department. Options include:
- Requesting a Lower Rate – Many providers offer self-pay discounts or adjusted rates for financial hardship.
- Setting Up a Payment Plan – Ask for interest-free installment options to manage high bills over time.
- Applying for Financial Assistance – Some hospitals provide charity care programs or discounts for uninsured patients. Providing proof of income or financial hardship can increase your chances of approval.
Billing Errors & Common Dispute Reasons
Medical billing errors are more common than many people realize, often leading to unexpected costs or insurance claim denials. Identifying these errors and understanding how to resolve them is essential to ensuring you only pay for legitimate charges.
Below, we outline the most frequent billing issues and the appropriate steps to correct them.
Read:
| Cardiology Medical Billing 101 |
| Orthopedic Medical Billing 101 |
| Radiology Medical Billing 101 |
| Orthotics Medical Billing 101 |
| Phsycian Medical Billing 101
|
Common Medical Billing Errors and How to Fix Them
Billing discrepancies can arise due to administrative mistakes, miscommunications, or coding errors. The most common billing issues include:
Duplicate Charges
A duplicate charge occurs when the same medical service appears multiple times on your bill, leading to an inflated total amount due. This can happen due to system errors, clerical mistakes, or accidental resubmissions by the provider.
How to Fix It:
- Compare your Explanation of Benefits (EOB) with the itemized bill.
- Contact the provider’s billing department for correction.
- Notify your insurer if the duplicate charge was processed.
Upcoding
Upcoding occurs when a provider bills for a more expensive procedure than what was actually performed. This can significantly increase your out-of-pocket costs and may even be considered fraudulent if done intentionally.
How to Fix It:
- Verify billing codes on your bill and EOB.
- Request medical records to confirm the actual procedure.
- Contact the provider for a code correction.
Incorrect Patient or Insurance Information
Mistakes in personal details, such as your name, insurance ID, or provider details, can lead to claim denials or incorrect billing amounts. These errors are often simple to correct but can cause significant delays in processing payments.
How to Fix It:
- Check that your name, policy number, and provider details are accurate.
- Request a corrected bill from your provider.
- Inform your insurer of any discrepancies.
Unbundling of Services
Unbundling happens when services that should be billed as a package are instead charged separately, resulting in a higher overall bill. This practice can increase costs unnecessarily, as bundled services are typically billed at a reduced rate.
How to Fix It:
- Request an itemized bill to check for unnecessary unbundling.
- Compare charges with standard billing codes.
- Ask the provider to rebundle the charges and issue a corrected bill.
If any errors are found, contact the provider’s billing department immediately. Request an itemized bill, compare it with your EOB, and submit supporting documents if needed.
How to Check If Your Medical Bill Is Accurate
Medical billing errors can lead to unnecessary charges. Here’s how to verify your bill before paying:
4 Easy Steps to Verify Your Medical Bill
- Request an Itemized Bill – Get a detailed breakdown of each charge.
- Compare It with Your EOB – Ensure the services and amounts match your insurance records.
- Check for Unexpected Charges – Identify duplicate charges or services you didn’t receive.
- Verify Provider and Service Details – Confirm the dates, provider name, and treatment details.
If discrepancies are found, contact the billing department immediately and request clarification or a correction. If unresolved, escalate the issue to your insurer or file a formal dispute.
What Are Surprise Medical Bills and How to Dispute Them?
Surprise medical bills occur when patients unknowingly receive out-of-network care, often during emergencies or at in-network facilities where some providers are not covered. The No Surprises Act protects patients by ensuring they are billed at in-network rates for covered situations.
If you receive a surprise bill, first confirm whether the No Surprises Act applies—if so, your insurer should process the bill at an in-network rate. If you’re still charged an out-of-network fee, file a dispute with your insurer for a formal review.
How to Request a Medical Bill Review from My Insurance
Submit a written request to your insurance company’s customer service or appeals department, citing errors or unjustified charges. Provide supporting documents and request a response within their required timeframe. If unresolved, escalate the issue to your state’s insurance commissioner.
Disputing medical bills requires persistence, documentation, and understanding your rights. By following the correct steps, you can successfully challenge incorrect charges and avoid unnecessary financial burdens.
Read:
| Why DME Suppliers Struggle with Reimbursements |
| The Biggest Billing Mistakes That Cost DME Providers Thousands |
| How to Appeal Denied Claims for Prosthetic Device Billing
|
How to File an Appeal for a Denied Medical Claim
- Review your policy and denial letter.
- Gather supporting documents (EOB, medical records, doctor’s notes).
- Write a detailed appeal letter.
- Submit your appeal within the insurer’s deadline.
- Follow up and escalate to state regulators if necessary.
How can I dispute medical bills in collections or without insurance?
To dispute medical bills in collections or without insurance:
- Validate the Debt: Request verification from the collection agency to confirm accuracy.
- Negotiate a Settlement: Contact the agency to arrange a payment plan or reduced amount.
- Seek Financial Assistance: Check for aid programs from healthcare providers or nonprofits.
How to Dispute Medical Bills on Your Credit Report?
Medical bills can harm your credit if reported inaccurately. To correct errors and protect your credit score, follow these steps:
Steps to Dispute Medical Bills on Your Credit Report:
- Check Your Credit Reports: Get copies from Equifax, Experian, and TransUnion to identify incorrect medical debts.
- Verify the Debt: Contact the medical provider or collection agency to confirm details and ensure accuracy.
- File a Dispute: If errors exist, dispute them with the credit bureaus online, by mail, or by phone, providing supporting documents.
- Follow Up: Credit bureaus must investigate disputes within 30 days and correct any verified errors.
Important Considerations:
- New Regulations (2025): The CFPB has banned medical bills from credit reports and restricted lenders from using them in lending decisions.
- Debts Under $500: Paid or small medical debts should not appear on credit reports—dispute them if they do.
- HIPAA Compliance: If personal medical data was mishandled during collections, you may file a HIPAA complaint.
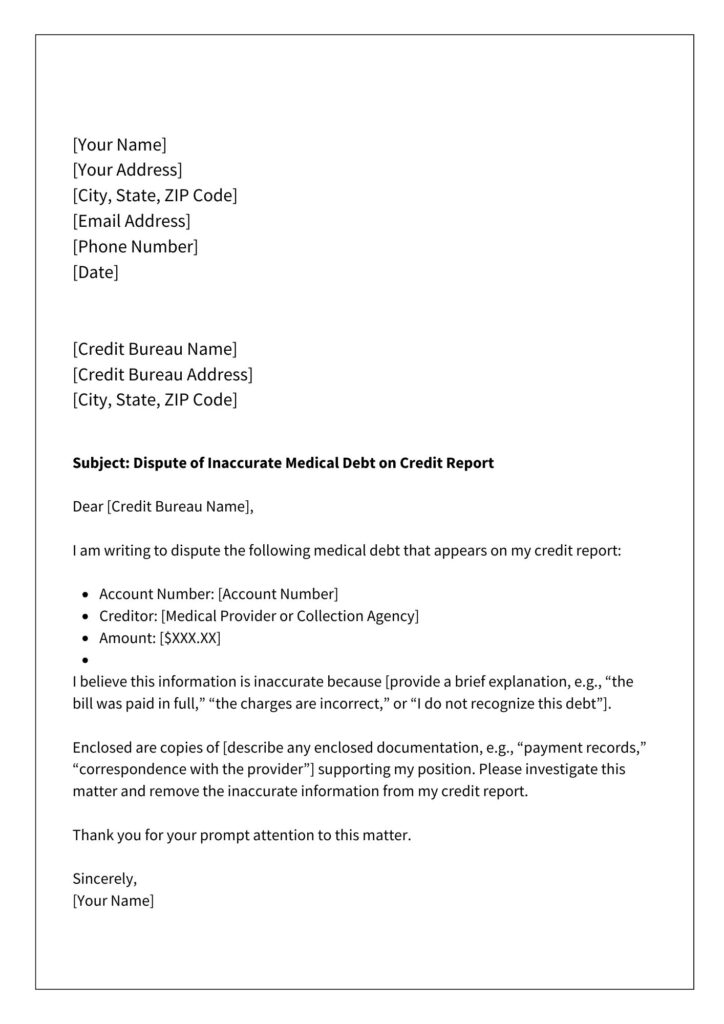
How to Dispute Medical Bills – Sample Letter
Frequently Asked Questions
How long do I have to dispute a medical bill?
You typically have 30 to 180 days to dispute a medical bill, depending on your insurance provider and state regulations. It’s important to check your insurance policy for specific time limits and submit your dispute as soon as possible to avoid delays or collection actions.
Can a medical bill go to collections if I dispute it?
Yes, a medical bill can still go to collections while you dispute it, but you have rights under the Fair Credit Reporting Act (FCRA) and the No Surprises Act to request a review and prevent unfair collection practices. Notify both your insurance company and the medical provider in writing to document the dispute and request a hold on collections.
How to request a medical bill review from my insurance?
To request a medical bill review, contact your insurance provider and ask for a claims review or reconsideration. Provide supporting documents such as your Explanation of Benefits (EOB), itemized medical bill, and proof of coverage. Submit your request in writing and follow up regularly to ensure your dispute is processed.
What is the No Surprises Act and How Does It Protect Me?
The No Surprises Act, effective January 2022, prevents patients from receiving unexpected out-of-network charges for emergency services, non-emergency care at in-network facilities, and air ambulance services. If you receive an unlawful charge, contact your insurance provider and reference the act.
Can a Medical Bill Go to Collections If I Dispute It?
Yes, but disputing a bill can delay collection actions. Notify both the provider and collection agency in writing that the bill is under dispute. The Fair Debt Collection Practices Act (FDCPA) protects you from unfair collection practices during this period.
What Are My Rights When Disputing a Medical Bill?
Under federal law, you have the right to request an appeal, receive an itemized bill, and dispute incorrect charges. The Affordable Care Act (ACA) also mandates insurers to provide reasons for claim denials.